Summer 2010 Collaborative Solutions Newsletter:
In this issue: Health Equity and Social Justice
The Center for Health Equity and Social Justice at the
Boston Public
Health Commission
Six key concepts
Community story: The Jamaica Plain Youth Health Equity Collaborative
Principles for Collaborative Solutions and Health Equity
What is new at Tom Wolff & Associates
The Center for Health Equity and Social Justice at the
Boston Public
Health Commission
For my Summer 2010 Newsletter, I’d like to tell you about the
work of the Center for Health Equity and Social Justice at the Boston
Public Health Commission. For the past five years, my work with this
center has been an especially exciting engagement. The simple fact
that a big U.S. city health department has an office named the Center
for Health Equity and Social Justice is surprising, and attests to
the exciting and cutting-edge vision that is being manifested by the
people in this organization. (http://www.bphc.org/programs/healthequitysocialjustice/Pages/Home.aspx)
I began my work with this innovative grassroots program when it was
called Boston REACH 2010 and was a CDC-funded initiative that focused
on racial disparities in breast and cervical cancer survival rates
for Black women in Boston. REACH, which stands for Racial and Ethnic
Approaches to Community Health, provides an excellent example of what
a community can accomplish when it acknowledges the issue of racism
in health and then creates a comprehensive social-change effort to
address inequalities. The outstanding quality of the work of Boston
REACH 2010 allowed the group under the skilled leadership of Nashira
Baril, Meghan Patterson, Courtney Boen and Erline Achille to continue
its work and to expand its scope. The REACH collaborative now receives
CDC funding as a Center of Excellence in the Elimination of Disparities.
In this capacity, the group has built on its initial accomplishments
and has also gone on to fund and support a large number of other communities
in New England that have followed their example and created community
responses to promote health equity.
All of these new efforts are built around the following key concepts:
1.
Addressing institutional and structural racism
The center has an explicit
approach to addressing institutional and structural racism. The Boston
Public Health Commission (BPHC) operates with the understanding that
racism is at the root of racial and ethnic health inequities. Racism
affects health directly by causing stress and anxiety, and it also
affects health indirectly by its impact on the social determinants
of health. Every community that receives a grant, following the lead
of the BPHC itself, engages in a three-day Undoing Racism workshop
(People’s Institute Undoing Racism and
Community Organizing Workshops™) for its core team and for community
members . The BPHC understanding of racism is based on the brilliant
work of Camara Phyllis Jones and her conception of levels of racism. http://www.scribd.com/doc/11917990/Racism-a-Gardeners-Tale.
2. Focus on social determinants of health
As the REACH 2010 group moved to become a Center of Excellence, they
also expanded their approach to include an explicit focus on the
social determinants of health. These social determinans are factors
that have an exceptionally strong and well-demonstrated influence
on health, such as education, socioeconomic status, housing, jobs,
economic opportunity, transportation, food access, safety, environmental
exposures, and so on. These aspects of life actually have a much
more profound impact on people’s overall health than does access
to health care. By looking at community health from the perspective
of the social determinants, groups can examine the ways in which
institutional racism plays out in each realm. As the powerful TV
series Unnatural Causes makes clear, your zip code
may be more important than your genetic code in determining your health (http://www.unnaturalcauses.org).
3. Grassroots community engagement
The center’s approach is
based on a core belief that grassroots involvement is essential to
solving problems. Barbara Ferrer, the Commissioner of Public Health
for the City of Boston, has this to say on the topic:
“The role
of a public health department is to create a space for residents to
come together to define a problem, to define the solutions, and then
enter into a dialogue with us—not the other way around. Not we
define the problem, we define the solution, and then we invite you
in to help us implement the solution, which is what we’re most
comfortable doing. We felt like part of the solution lay in being able
to get a broad-based coalition that would tackle issues like racism.
And that would bring together the provider community with the resident
community to tackle those issues.” (In “Creating
a Health Equity Coalition: Lessons from REACH Boston 2010,” Boston Public
Health Commission, 2010.)
4. Policy change
The project has an explicit focus on creating long-lasting
policy and social change that will endure as a legacy in each participating
community. This follows the lead of the CDC’s new director, Tom
Frieden (see his “A Framework for Public Health Action.”2010). With
this intention in mind, the approach goes beyond creating better understandings
of health disparities and new programs. It also insists that communities
explore policy changes that will improve community health. Examples
include zoning changes to allow for construction of a new supermarket
in a low-income community, or advocating with the legislature to find
summer jobs for teens. All grant-recipient communities are required
to develop and implement policy-based solutions for addressing racism
and the social determinants of health.
5. Focus on a shift from social service to social change
For traditional
nonprofit agencies that work with the center, the greatest challenge
often is found in the explicit shift in focus from social service to
social change. The center is not interested in the creation of new
education programs for Black men at risk of diabetes. Instead, it wants
to promote efforts that will change the institutional racism in housing,
food access,and employment policies that put Black men at higher risk
for diabetes. The goal is to prevent the illness, not provide palliative
treatment. For nonprofits accustomed to delivering social services,
this is a huge change in emphasis.
6. Collaboration
Finally, the center understands that in order to
accomplish systems changes of this large scope a community must
develop a broad-based coalition of residents and agencies that will
work together collaboratively.
Together these six key concepts become a powerful force for transformative
community change.
A new manual describing the work of the BPHC Center
for Health Equity and Social Justice will be available later this summer.
I have had the honor of co-authoring this publication, and it gives
me great joy to be part of this acknowledgment of the center’s trailblazing
work and to put its accomplishments in a form that will help even more
communities achieve health equity. Entitled Creating a Health Equity
Coalition: Lessons from REACH Boston 2010, the manual will be available
at http://www.bphc.org/programs/healthequitysocialjustice/toolsandreports/
Pages/Home.aspx
Another view of this transformative work is available now at :
http://www.youtube.com/watch?v=TCnDZW-sJXU
References:
Jones, Camara Phyllis. “Levels
of Racism: A Theoretic Framework and a Gardener’s Tale.” American
Journal of Public Health 90, no. 8 (August 2000): 1212–1215. http://www.scribd.com/doc/11917990/Racism-a-Gardeners- Tale.
Frieden, Thomas R. “A Framework for Public Health Action: The
Health Impact Pyramid.” American
Public Health Journal 100, no.
4 (April 2010): 590–595.
Community Story: The Jamaica Plain Youth Health Equity Collaborative
What does support of other communities by the center look like? I’d
like to make the model concrete by telling the story of one local coalition
that is being supported by the center. Jamaica Plain (JP) is a fascinating
neighborhood in Boston. It includes an affluent white community
along with low-income Black and Latino communities — there are
really two JPs, the rich one and the poor one. Accompanying this economic
division are social, and health, inequities. To address the gap, the
Southern JP Health Center has become the sponsor for the development
of the Jamaica Plain Youth Health Equity Collaborative.
The collaborative chose to focus on youth for two big reasons: a strong
base of agencies working with young people already existed, and the
group understood that youth issues are inseparable from community and
family issues. By centering their efforts on health equity for young
people, the group was able to narrow its field of attention (but not
much).
The group’s guiding concept, based on a framework that takes
into account the social determinants of health, envisions the following
life qualities for healthy youth in JP:
- They have high-quality education that helps them achieve their
dreams
- They have meaningful living -wage jobs
- They live in a safe and connected community environment
- They live in high-quality and affordable housing
- They are engaged in high-quality and comprehensive health care
- They have access to high-quality food and an environment that promotes
physical activity
The goals for the JP Youth Health Equity Collaborative were to:
- Involve residents, organizations, and youth
- Examine health disparities
- Identify causes, including social determinants
- Create a common language and framework
- Define and implement programs and change policies
The collaborative is led by a remarkably skilled organizer, Abigail
Ortiz, in partnership with many local agencies that have made a serious
commitment to ensuring that this collaborative succeeds.
In its first year of planning, the collaborative held a series of
interactive Youth Health Equity meetings, called “bucket meetings.” Each
bucket meeting involved a cluster of young people and focused on one
social determinant of health. The purpose of the meetings was to gather
youth perceptions on that social determinant of health. Collaborative
members presented each small group of young people with a case example;
the examples were variations on real stories about community members.
Here’s the type of story the young people were asked to consider: “Claudia
is 16 and living with her mom in public housing in JP. She has been
trying unsuccessfully for two years to get a job. She is always turned
down. She is getting discouraged, and spends more time watching TV
and with her boyfriend who is dealing weed.” The facilitators
then asked the small discussion groups the following questions:
- What are the employment inequities for low-income African American/Latino
youth illustrated by this story?
- What is the role of institutional racism in Claudia’s not
getting a job?
- How will this affect Claudia’s health? I.e., what are the
health impacts of the job situation for low-income African American/Latino
youths?
- And what could we do about this? What possible action steps and
strategies come to mind?
The ”bucket meetings” were well attended by JP young people,
who had no difficulty addressing these questions for each bucket. Young
members of the community implicitly understand the issue of social
determinants of health and institutional racism.
 Following the bucket meetings, the collaborative held a Youth Retreat.The
more than 20 young people who participated chose jobs as the ”bucket” area
that they wanted to address first. During the retreat, facilitators
asked the young people to indicate which JP institutions affect the
health of a typical JP youth. As these organizations were mentioned,
they were put on a list. When the list was complete, the facilitators
wrote each named institution on a sheet of paper and asked the young
participants to rate each entity, using colored dots, as being supportive of the health of JP youth, detrimental to their health, or neutral.
The group then stepped back to view the whole and engaged in a discussion
of the map of institutional racism in JP that they had created.
Following the bucket meetings, the collaborative held a Youth Retreat.The
more than 20 young people who participated chose jobs as the ”bucket” area
that they wanted to address first. During the retreat, facilitators
asked the young people to indicate which JP institutions affect the
health of a typical JP youth. As these organizations were mentioned,
they were put on a list. When the list was complete, the facilitators
wrote each named institution on a sheet of paper and asked the young
participants to rate each entity, using colored dots, as being supportive of the health of JP youth, detrimental to their health, or neutral.
The group then stepped back to view the whole and engaged in a discussion
of the map of institutional racism in JP that they had created.
Since those initial, clarifying meetings, the JP Youth Health Equity
Collaborative has been hard at work addressing the issue of jobs for
young people. First, the collaborative has organized a series of work
groups on multiple aspects of youth employment:
- Job development,
- Creating a youth entrepreneurship business, and job training.
- Communications
 As part of the collaborative’s work on youth jobs, the group
helped plan and took part in a youth-led protest rally at the State
House urging the legislature to reinstate funds for summer jobs for
young people. The orderly yet powerful rally of 700 young people caught
the attention of both the media and the legislators.
As part of the collaborative’s work on youth jobs, the group
helped plan and took part in a youth-led protest rally at the State
House urging the legislature to reinstate funds for summer jobs for
young people. The orderly yet powerful rally of 700 young people caught
the attention of both the media and the legislators.
Finally, the project issued a report on health in young people in
JP. Titled “02130 Health and Youth,” it has a picture of
a “teeny” on the cover and the phrase, “If you know
what this is, this report is for YOU.” A “teeny” is
a drink that contains no positive nutritional value—it’s
just sugar, water, and coloring. It is readily available in the stores
that cater to African-American and Latino youth. Stores in the white
neighborhoods of JP sell fresh juice instead.
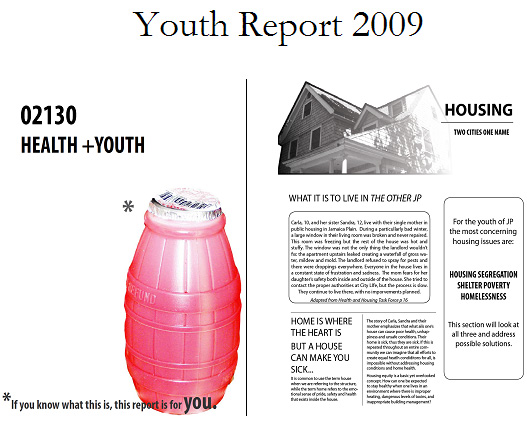
Thus the “teeny” is
a great symbol of the health inequity campaign. Inside the report,
each social determinant is examined, and the coverage includes youth
stories, youth quotes, data, and ideas on what actions can be taken.
The report, authored by Meghan Wood, is available on the BPHC web site: http://www.bphc.org/programs/healthequitysocialjustice/toolsandreports/
Pages/Home.aspx
Priority areas and key principles
I have recently been struck with how similar the priority areas of
the Center for Health Equity and Social Justice are to the six key
principles I’ve written about in The Power of Collaborative
Solutions.
The center’s work illustrates the six key principles in action.
Let me demonstrate, using examples from some of the center’s
communities that I have had the privilege of working with:
Principles
for Collaborative Solutions and Health Equity
1.Encourage true collaboration as the form of exchange.
The relationship
between the Boston Public Health Commission and the community coalitions,
as articulated by Barbara Ferrer and enacted in the coalition activities,
is truly at the level of collaboration where all participants are “enhancing
the capacity of the other.
2. Engage the full diversity of the community, especially
those most directly affected.
The JP Youth Health Equity Collaborative certainly illustrates having
those most affected by the issues (the JP youth of color) at the table
and setting the agenda.
3. Practice democracy and promote active citizenship
and empowerment.
The Boston REACH coalition begins its meetings by
going around the room with introductions, during which all members
say their names and their neighborhoods. This reflects a conscious
decision to put all members on equal footing and to eliminate fancy
titles and institutions as part of the introductions. In addition,
the Boston REACH Coalition is co-chaired by two community members,
who get coaching and training to guarantee their success in their roles
in collaborating with each other and in guiding the rest of the group
in collaboration.
4. Employ an ecological approach that builds on community
strengths.
The whole approach, emphasizing the social determinants of
health and operating through bucket meetings, is designed to help residents
understand their health in the context of their environment. The success
of this approach becomes clear when women note that the meetings bring
them a sense of huge relief, because they previously always felt that
everyone was blaming them for being the cause of their own illness.The
tag line that your zip code may be more important than your genetic
code in determining your health is the best line I have ever heard
for explaining an ecological approach.
5. Take action by addressing
issues of social change and power on the basis of common vision.
In
Springfield, Massachusetts, the local project is focused on health
equity and food access. Here one major area of attention has involved
zoning changes that will permit the opening of a supermarket in the “food
desert” of the Mason Square area of Springfield.
6. Engage spirituality
as your compass for social change.
I began my work with BPHC by working
with the Boston REACH Coalition when its focus was limited to the incidence
and treatment of breast and cervical cancer in Black women in Boston.
The group of women who worked on leadership, team building, and sustainability
with me were passionate, caring, and committed to making a difference
in their community. They epitomize the spiritual principles of acceptance,
appreciation, deep compassion and interdependence. I am so grateful
to have had the opportunity to know and work with them.
What is New at Tom Wolff & Associates
The release of The Power
of Collaborative Solutions has meant a busy time here at Tom Wolff
and Associates! I’ve been doing book presentations
and signings large and small, and love meeting with people and talking
about collaborative solutions. I was invited to present at the Canadian
Community Psychology Conference in Ottawa in May, and I also held a
book signing there. Then in June I facilitated a two-day workshop on
collaborative solutions for the Third International Community Psychology
Conference, held in Puebla, Mexico.
In the coming months, I’ll be doing talks and readings in, among
other places, Madison Wisconsin; San Diego; Los Angeles (as part of
a Presidential Panel at the APA Convention); Brattleboro,Vermont; Milwaukee,Wisconsin;
and locally here in Massachusetts. Being able to share my experience
with people through the medium of a book release is certainly a learning
experience for me, and I’m enjoying it.
Many of the individual readers I have talked with have made special
mention of the book’s emphasis on spirituality, and how refreshing
and helpful they find that to be. It took a leap of faith to include
the material in the manuscript, because I wasn’t sure how it
would be received. However, to leave it out would have been to overlook
an essential part of community-building for all of us. The role of
spirituality in social change is the area that I hope to spend most
time examining over the coming years.
I have been very pleased to hear from many of my academic colleagues
that they will be adopting The Power of Collaborative Solutions for
their course offerings in the fall. This is happening not only across
the United States but also in Canada, Puerto Rico, and Portugal. I
couldn’t be happier to hear of the widespread enthusiasm for
the book as a resource for students, as well as professionals, around
the world. With enough of us involved, we can build healthy communities,
from the ground up, across the globe.
More information on The
Power of Collaborative Solutions is available
at www.tomwolff.com.
